Healthcare staffing challenges continue to prevail in 2022. The COVID-19 pandemic has impacted how healthcare organizations manage their revenue cycle. Staffing shortages mean that providers are forced to hire inexperienced billing staff, increasing the practices’ time spent in accounts receivable (AR) and resulting in a loss of revenue.
How can providers automate their front office to increase workflow efficiencies, maximize payouts, and increase profitability? By using a service to automate revenue cycle management.
What Is Revenue Cycle Management and Why Does It Matter?
Revenue cycle management (RCM) is a service that automates the process used to track payment collections for the rendering of health services, from scheduling the initial appointment to ensuring that all payments are collected from both patients and third-party payers. Physicians can shorten the time spent in accounts receivable, maximize reimbursements, and increase revenue by employing the use of RCM. Put simply, RCM allows medical practices to come out from financial stress, continue to make a profit, and keep their doors open.
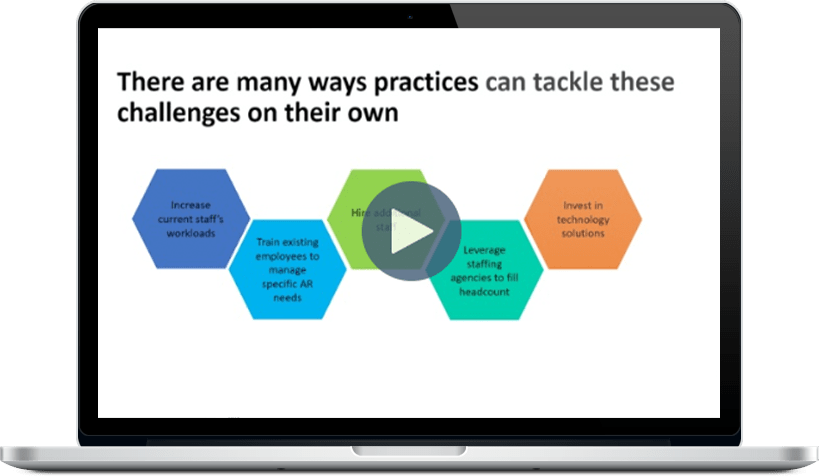
A recent MGMA study sheds light on how medical practices have seen their time in accounts receivable (AR) change in 2021. Nearly half (49%) of medical practices polled reported an increase in time in AR, compared to just 15% that reported a decrease. Practices that reported an increase in time in AR shared themes of either being short-staffed or experiencing steep learning curves for new billing staff.
Practices that reported a decrease in time in AR attribute this to either outsourcing components of their revenue cycle management or implementing new artificial intelligence/machine learning tools to streamline redundant tasks.
What Are the Benefits of Revenue Cycle Management?
RCM leverages professionals and medical billing software to gain statistical insights to unveil, monitor, and call to action milestones within a claim’s life cycle journey. Working with an RCM service enhances timeliness and streamlines patient and third-party communication to drive revenue growth for practices. Some of the main benefits of using RCM include:
- Faster eligibility verification: The ability to verify a patient’s insurance information and coverage before their appointment improves the patient experience.
- Expedited and accurate claims submissions: RCM emphasizes the accuracy of patient information and coding so that claims are paid after the first submission.
- Reduction in claims denial rates: When claims are accepted, doctors and staff don’t have to spend time investigating and appealing the denial.
- Decreased burden on administrative staff: RCM streamlines front-end tasks, allowing administrative staff to work more efficiently.
- Ability to focus on quality patient care: When a practice streamlines its administrative tasks, it can put more time and energy into providing patient-centered care.
The benefits of partnering with a revenue cycle management service affect both healthcare providers and their patients.
Empower Your Front-End Office
Whether you’re a small clinic without a billings department or are generally looking to optimize business operations, partnering with an RCM service can help your medical practice manage administrative services to maximize the efficiency of your existing team, therefore resulting in increased revenue and allowing you to keep your doors open.
Sources:
https://www.medicaleconomics.com/view/mgma-practices-still-struggling-with-staffing-challenges
https://www.youtube.com/watch?v=mUAR_qNrdFg
https://mgma.com/resources/resources/revenue-cycle/not-so-graceful-aging-half-of-practices-saw-days-i